What Causes Varicose Veins?
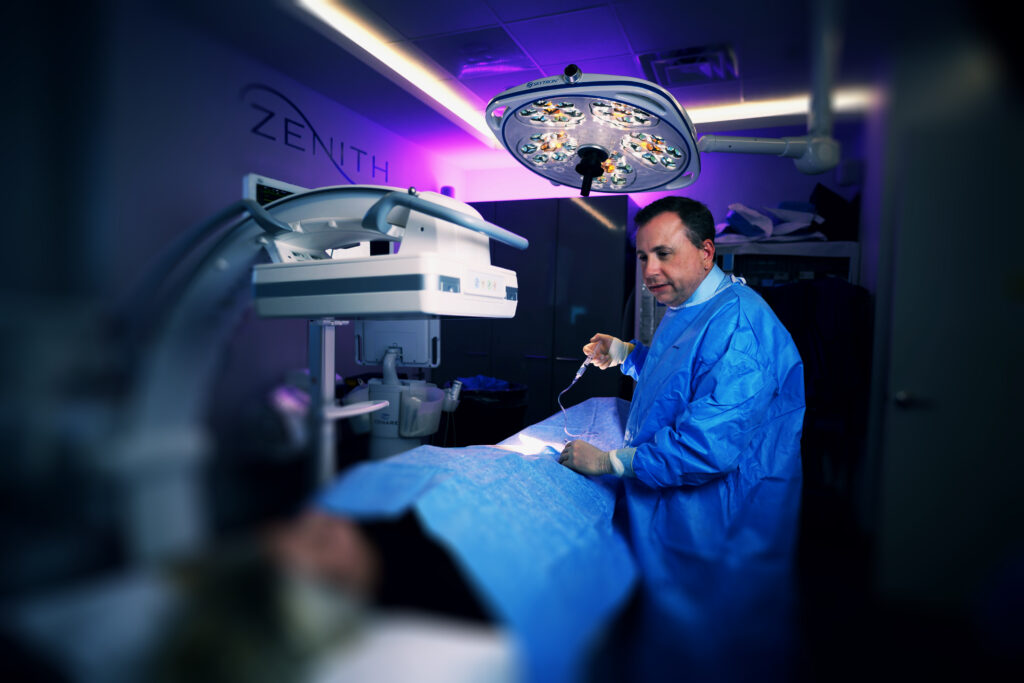
Has it started to feel like the veins on your legs are becoming more noticeable or even painful? Varicose veins are common but often uncomfortable. At Zenith Vascular & Fibroid Center, we proudly offer a range of varicose vein treatment options. Learn more during a consultation with us in Memphis, TN!

What Are Varicose Veins?
Varicose veins are swollen, twisted veins that are often blue or dark purple in color. They usually occur in the legs, but can also develop in other parts of the body. Varicose veins are a common condition that affects many people, and are more common in women than in men.
Varicose veins occur when the valves in the veins that help to keep blood flowing towards the heart become weakened or damaged. This can cause blood to pool in the veins, which can lead to swelling, bulging, and a twisted appearance. In addition to their unsightly appearance, varicose veins can also cause symptoms such as aching, throbbing, and heavy or tired legs.
Risk factors for varicose veins include age, genetics, pregnancy, obesity, and a sedentary lifestyle. Treatment options for varicose veins include lifestyle changes such as exercise and weight loss, compression stockings, and medical procedures such as sclerotherapy, laser therapy, and vein surgery.

How Does a doctor diagnose varicose veins
A doctor can diagnose varicose veins by conducting a physical exam and reviewing your medical history. During the physical exam, the doctor will look for any visible signs of varicose veins, such as swollen, twisted, or bulging veins. They may also ask you questions about any symptoms you may be experiencing, such as pain, swelling, or aching in the affected area.
In some cases, the doctor may also recommend additional tests to confirm the diagnosis or to check for any underlying conditions. These tests may include:
1. Duplex ultrasound: This is a non-invasive test that uses sound waves to create images of the veins in your legs. This test uses high-frequency sound waves to create images of the veins and the blood flow within them. By combining traditional ultrasound imaging with Doppler technology, the test can provide a detailed picture of the structure and function of the veins, including the presence of any blockages or abnormalities.
During the test, a technician will apply a gel to the affected area and use a handheld device called a transducer to generate images of the veins on a computer screen. The technician will also use the Doppler technology to measure the speed and direction of blood flow within the veins. This information is used to evaluate the severity of any underlying venous insufficiency and to plan appropriate treatment.
2. Venogram: This is an imaging test that involves injecting a contrast dye into your veins and taking X-rays to see how the blood is flowing through your veins. A venogram is typically used in cases where other non-invasive diagnostic tests such as ultrasound have not provided a clear picture of the veins.
3. CT scan or MRI: These imaging tests may be used to get a more detailed view of your veins and to check for any underlying conditions that may be contributing to your varicose veins.
Treatment of Varicose Veins
Treatment for varicose veins depends on the severity of the condition. In mild cases, the doctor may recommend lifestyle changes such as regular exercise, weight loss, and avoiding prolonged standing or sitting. In more severe cases, the doctor may recommend one of the following treatment options:
1. Endovenous laser treatment (EVLT): This is a minimally invasive procedure that uses laser energy to seal off the affected vein.
Endovenous laser treatment (EVLT) is a minimally invasive procedure used to treat varicose veins. During the procedure, a thin laser fiber is inserted into the affected vein through a small incision. Once the fiber is in place, laser energy is applied to the inside of the vein, causing it to heat up and close off. The body then naturally redirects blood flow to healthier veins, relieving symptoms and improving the appearance of the affected area.
EVLT is typically performed on an outpatient basis, meaning the patient can go home the same day. It is generally well-tolerated and has a high success rate. The procedure typically takes less than an hour to complete and requires only local anesthesia. EVLT is often preferred over traditional vein stripping surgery because it is less invasive, has fewer side effects, and requires less downtime for recovery. However, it is important to discuss the risks and benefits of any treatment with a qualified healthcare professional.
2. Sclerotherapy: This is a non-surgical treatment that involves injecting a solution directly into the affected vein, causing it to collapse and eventually fade away.
Sclerotherapy is a medical procedure used to treat varicose veins and spider veins. The procedure involves injecting a solution directly into the affected veins, which causes them to scar and eventually close off. Blood flow is then naturally redirected to healthier veins, improving the appearance of the affected area and reducing symptoms such as pain, swelling, and cramping.
The solution used in sclerotherapy is usually a saline solution or a chemical solution, such as sodium tetradecyl sulfate or polidocanol. The solution irritates the inner lining of the vein, causing it to swell and stick together. Over time, the vein is absorbed by the body and disappears.
Sclerotherapy is typically performed on an outpatient basis, meaning the patient can go home the same day. The procedure is usually well-tolerated and has a high success rate, although multiple treatments may be necessary for optimal results. Sclerotherapy is often preferred over more invasive procedures because it is less painful, requires no downtime for recovery, and
3. Vein Stripping and Ligation: This is a surgical procedure that involves making incisions in the skin and tying off or removing the affected vein.
4. Ambulatory Phlebectomy: This is a minimally invasive surgical procedure that involves removing the affected vein through small incisions in the skin. During the procedure, the surgeon makes small incisions in the skin and removes the affected vein through the incisions. Ambulatory phlebectomy is typically performed using local anesthesia, which numbs the area around the vein and allows the patient to remain awake during the procedure. Ambulatory phlebectomy is considered a safe and effective procedure, with a high success rate and low risk of complications.
5. Radiofrequency Ablation: This is a minimally invasive procedure used to treat varicose veins. During the procedure, a thin catheter is inserted into the affected vein and radiofrequency energy is used to heat and seal the vein. This causes the vein to collapse and eventually be reabsorbed by the body. RFA is typically performed using local anesthesia and is a same-day outpatient procedure. RFA is often used to treat larger varicose veins and has been shown to be effective in reducing symptoms such as pain, swelling, and leg fatigue.
Your doctor will determine the best treatment option. It is important to note that while these procedures can effectively remove varicose veins, they do not guarantee that new varicose veins will not develop in the future.
After the Varicose Vein Treatment
The recovery process after varicose vein treatment can vary depending on the type of treatment performed. In general, after treatment, patients are advised to avoid strenuous physical activity and to rest as much as possible. They may also be advised to wear compression stockings to promote healing and reduce swelling.
After a minimally invasive treatment like endovenous laser therapy (EVLT) or radiofrequency ablation (RFA), patients can typically return to normal activities the day after the procedure. However, they may have to avoid heavy lifting or strenuous exercise for a few days.
After a surgical procedure like vein stripping or ligation, recovery may take a bit longer. Patients may need to take a few days off work and avoid strenuous physical activity for several weeks. They may also need to wear compression stockings for a longer period of time.
In both cases, patients are typically advised to maintain a healthy lifestyle to prevent the recurrence of varicose veins. This may include regular exercise, maintaining a healthy weight, and avoiding prolonged periods of sitting or standing.
Varicose Veins and Pregnancy
Pregnant women are more likely to develop varicose veins due to the increased pressure on the veins in the lower body caused by the growing uterus. As the uterus expands, it puts pressure on the inferior vena cava, a large vein that carries blood from the lower body to the heart. This pressure can slow down the blood flow in the veins of the legs and feet and cause the veins to expand and become more visible. Additionally, hormonal changes during pregnancy can also contribute to the development of varicose veins. The hormone progesterone, which helps to relax the smooth muscles in the uterus, can also relax the walls of the veins, making them more prone to pooling of blood and swelling. Furthermore, pregnancy can also lead to an increase in blood volume, which can put additional pressure on the veins. These factors combined make pregnant women more susceptible to varicose veins.
Did You know? Pregnancy is a common risk factor for varicose veins, with up to 40% of pregnant women developing the condition. (Source: American Pregnancy Association)
Doctor’s Recommendations
The treatment of varicose veins depends on the severity of the condition. Here are some common suggestions that doctors may give to patients with varicose veins:
1. Lifestyle changes: Doctors may suggest that patients make certain lifestyle changes to help manage their varicose veins. This may include losing weight, avoiding prolonged periods of sitting or standing, and engaging in regular exercise to promote healthy blood flow.
2. Compression Stockings: Compression stockings are a common treatment for varicose veins. These stockings help to improve blood flow by applying pressure to the legs, which can reduce swelling and discomfort.
3. Sclerotherapy: This is a minimally invasive procedure in which a solution is injected into the affected veins to cause them to shrink and eventually disappear.
4. Endovenous Laser Treatment: This procedure involves the use of laser energy to heat and close off the affected veins.
5. Surgery: In severe cases, surgery may be necessary to remove or repair damaged veins.
It’s important to note that the treatment plan for varicose veins will depend on the individual.
