How Is Peripheral Artery Disease Treated – Memphis TN
Leg cramping and pain or heaviness in the legs? These are just a few common symptoms of PAD. At Zenith Vascular & Fibroid Center, we proudly offer a range of vascular treatment options. Continue reading for learn more about Peripheral Artery Disease, it’s risk factors, and treatment options. Learn more during a consultation with us in Memphis, TN!


What is peripheral artery disease?
Peripheral Artery Disease (PAD) is a condition that affects the blood vessels outside of the heart and brain, primarily the arteries that supply blood to the limbs, most commonly the legs. It occurs when the arteries become narrowed or blocked due to a buildup of fatty deposits called plaque. This narrowing or blockage restricts blood flow to the affected areas, leading to various symptoms and potential complications.
Common symptoms of PAD include pain, cramping, or aching in the legs, particularly during physical activity or walking (known as intermittent claudication). Other signs may include numbness, weakness, or a cold sensation in the legs or feet. In severe cases, PAD can lead to non-healing wounds or ulcers, tissue damage, and even limb amputation.
Several risk factors contribute to the development of PAD, including smoking, diabetes, high blood pressure, high cholesterol, obesity, and a family history of the disease. Age and a sedentary lifestyle are also associated with a higher risk.
Early diagnosis and management of PAD are crucial to prevent further complications. Treatment options may include lifestyle modifications such as regular exercise, a healthy diet, smoking cessation, and medication to control underlying conditions. In more severe cases, procedures like angioplasty or bypass surgery may be necessary to restore blood flow to the affected areas.
If you suspect you may have symptoms of PAD, it is important to consult with a healthcare professional for an accurate diagnosis and appropriate treatment plan.

What are some symptoms of Peripheral Artery Disease?
Peripheral Artery Disease (PAD) often presents with a range of symptoms, which primarily occur due to reduced blood flow to the limbs. Common symptoms of PAD include:
1. Pain or discomfort in the legs: This is one of the most common symptoms of PAD. The pain is often described as cramping, aching, or a feeling of heaviness in the legs, particularly during physical activity. This pain, known as intermittent claudication, typically improves with rest.
2. Numbness or weakness: Some individuals with PAD may experience numbness, weakness, or a tingling sensation in the legs or feet.
3. Coldness or changes in skin color: Reduced blood flow can cause the affected limb to feel colder than usual, and the skin may appear pale or bluish in color.
4. Slow-healing wounds: PAD can impair the body’s ability to heal wounds, leading to ulcers or sores that take a long time to heal. In severe cases, these wounds may become infected.
5. Hair loss or slow hair growth: Reduced blood flow can result in decreased hair growth or even complete hair loss on the legs and feet.
6. Weak or absent pulses: A healthcare professional may detect weak or absent pulses in the affected limb during a physical examination.
7. Erectile dysfunction (in men): PAD can affect the blood flow to the penile arteries, leading to difficulties in achieving or maintaining an erection.
It is important to note that some individuals with PAD may not experience any symptoms, especially in the early stages. However, if you have any concerns or experience any of the aforementioned symptoms, it is advisable to consult a healthcare professional for a proper evaluation and diagnosis. Reach out to our vascular health professions at Zenith Vascular & Fibroid Center for a consultation.
What can cause Peripheral Artery Disease?
Peripheral Artery Disease (PAD) is primarily caused by atherosclerosis, a condition characterized by the buildup of plaque within the arteries. This plaque is composed of cholesterol, fatty deposits, calcium, and other substances that accumulate on the inner walls of the arteries, narrowing them and reducing blood flow. The following factors contribute to the development of PAD:
1. Smoking: Smoking is a significant risk factor for PAD as it damages the arteries and promotes the formation of plaque.
2. Diabetes: High blood sugar levels associated with diabetes can damage the lining of blood vessels, leading to the development of atherosclerosis.
3. High blood pressure: Uncontrolled hypertension causes wear and tear on the arterial walls, making them more susceptible to plaque buildup.
4. High cholesterol levels: Elevated levels of LDL (bad) cholesterol and low levels of HDL (good) cholesterol contribute to the accumulation of plaque in the arteries.
5. Obesity: Being overweight or obese increases the risk of developing atherosclerosis and PAD due to the strain placed on the cardiovascular system.
6. Sedentary lifestyle: Lack of regular physical activity weakens the cardiovascular system and promotes the development of atherosclerosis.
7. Age: The risk of PAD increases with age, as the arteries naturally become less flexible and more prone to plaque buildup.
8. Family history: Having a family history of PAD or other cardiovascular diseases may indicate a genetic predisposition to developing the condition.
9. Ethnicity: Certain ethnic groups, such as African Americans and Hispanics, have a higher prevalence of PAD.
It is important to note that while these factors contribute to the development of PAD, they do not guarantee that an individual will develop the condition. However, adopting a healthy lifestyle, managing underlying risk factors, and seeking regular medical care can significantly reduce the likelihood of developing PAD.

How is Peripheral Artery Disease diagnosed?
Peripheral Artery Disease (PAD) can be diagnosed through a combination of medical history evaluation, physical examination, and diagnostic tests. The following are common methods used to diagnose PAD:
1. Ankle-Brachial Index (ABI): This non-invasive test compares the blood pressure in the ankle with the blood pressure in the arm to assess the presence and severity of PAD. A lower ABI value indicates reduced blood flow to the legs.
2. Doppler Ultrasound: This test uses sound waves to assess blood flow in the arteries and determine any blockages or narrowing. It can help identify the location and severity of arterial obstruction.
3. Angiography: This invasive procedure involves injecting a contrast dye into the arteries and taking X-ray images to visualize the blood flow and identify any blockages.
4. Magnetic Resonance Angiography (MRA): MRA is a non-invasive imaging technique that uses magnetic fields and radio waves to produce detailed images of the blood vessels. It can provide information about the location and severity of arterial blockages.
5. Computed Tomography Angiography (CTA): CTA combines X-ray images and computer technology to create detailed 3D images of the blood vessels. It helps identify areas of arterial narrowing or blockages.
6. Blood Tests: Blood tests may be conducted to check for risk factors associated with PAD, such as cholesterol levels, blood sugar levels (for diabetes), and markers of inflammation.
Early diagnosis of PAD is essential for effective management and to prevent complications. If you have concerns about PAD, contact us to consult with our healthcare professionala for a comprehensive evaluation and appropriate testing.
How Is Peripheral Artery Disease Treated?
There are various treatment options available for Peripheral Artery Disease (PAD), and the choice of treatment depends on the severity of the condition and individual patient factors. The primary goals of PAD treatment are to manage symptoms, improve blood flow, prevent further progression, and reduce the risk of complications. Some common treatment approaches for PAD include:
1. Lifestyle Modifications: Making healthy lifestyle changes is often the first step in PAD management. This may include regular exercise, adopting a healthy diet, quitting smoking, managing weight, and controlling other risk factors such as high blood pressure, high cholesterol, and diabetes.
2. Medications: Medications may be prescribed to help manage PAD symptoms and reduce the risk of complications. This can include medications to lower cholesterol, control blood pressure, prevent blood clots, and manage diabetes.
3. Exercise Therapy: Supervised exercise programs, such as supervised walking or treadmill exercise, can help improve symptoms and increase walking distance by promoting collateral blood vessel formation.
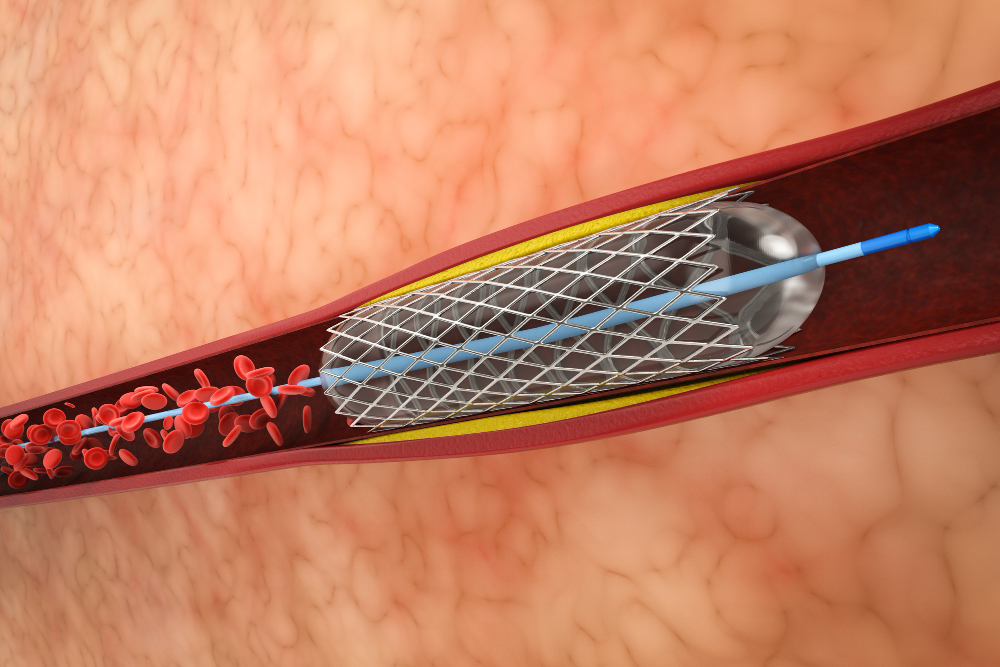
4. Angioplasty and Stenting: In cases where there are significant blockages in the arteries, minimally invasive procedures like angioplasty and stenting may be performed. Angioplasty involves inflating a small balloon in the blocked artery to widen it, and a stent may be placed to keep the artery open.
5. Bypass Surgery: In more severe cases, bypass surgery may be recommended to create a new pathway for blood flow by using a graft to bypass the blocked or narrowed artery.
6. Amputation: In extreme cases where severe PAD has led to tissue damage or non-healing ulcers, amputation of the affected limb may be required as a last resort.
The choice of treatment will depend on the individual patient’s condition, overall health, and other factors. It is important to consult with a healthcare professional to determine the most appropriate treatment plan for your specific situation.
Early detection and management of PAD can significantly improve outcomes and reduce the risk of complications. Regular follow-up with healthcare providers is crucial for monitoring the condition and adjusting the treatment plan as needed.

What Happens After The Peripheral Artery Disease Treatment
After undergoing treatment for Peripheral Artery Disease (PAD), the specific outcome and follow-up care will depend on the type of treatment received and the individual patient’s response. Here are some general aspects to consider:
1. Symptom Improvement: Treatment aims to alleviate symptoms associated with PAD, such as leg pain, cramping, or numbness. Many patients experience significant improvement in their symptoms after treatment, allowing them to engage in physical activities with less discomfort.
2. Enhanced Blood Flow: Treatment interventions like angioplasty, stenting, or bypass surgery aim to restore or improve blood flow to the affected limbs. This can lead to better oxygen and nutrient supply to the tissues, promoting healing and reducing the risk of complications.
3. Rehabilitation: In some cases, patients may undergo a rehabilitation program after PAD treatment. This may involve supervised exercise therapy to gradually increase walking distance and improve overall cardiovascular fitness. Rehabilitation can help patients regain strength, endurance, and mobility.
4. Medication Management: Depending on the underlying risk factors and individual patient needs, medication management may continue after PAD treatment. This can include medications to control blood pressure, lower cholesterol, prevent blood clots, or manage diabetes. Regular follow-up appointments with healthcare providers are important to monitor the effectiveness of medications and adjust the treatment plan if necessary.
5. Lifestyle Modifications: Regardless of the treatment received, adopting and maintaining a healthy lifestyle is crucial in managing PAD. This includes making dietary changes, engaging in regular exercise, quitting smoking, managing weight, and controlling other risk factors. Lifestyle modifications can help improve overall cardiovascular health and reduce the risk of further complications.
6. Follow-Up Care: After treatment, regular follow-up visits with your healthcare provider are essential. They will monitor your progress, assess the effectiveness of treatment, and make any necessary adjustments to your care plan. Ongoing monitoring is important to detect any potential recurrence or progression of PAD and to address any new concerns that may arise.
Doctors Recommend to patients who had Peripheral Artery Disease
After a diagnosis of Peripheral Artery Disease (PAD), we typically recommend a combination of lifestyle modifications, medication management, and potentially, interventional procedures. Here are some common recommendations for patients with PAD:
1. Lifestyle Modifications: Lifestyle changes play a crucial role in managing PAD. Doctors often advise patients to:
- Quit smoking: Smoking cessation is vital as it significantly improves symptoms, slows disease progression, and reduces the risk of complications.
- Adopt a healthy diet: A heart-healthy diet low in saturated fats, cholesterol, and sodium is recommended. It should include a variety of fruits, vegetables, whole grains, lean proteins, and healthy fats.
- Engage in regular exercise: Supervised exercise programs, such as walking or other low-impact activities, are often prescribed to improve walking distance, reduce symptoms, and enhance overall cardiovascular health.
- Manage weight: Maintaining a healthy weight can help reduce stress on the arteries and improve blood flow.
2. Medication Management: Doctors may prescribe medications to address underlying risk factors and manage symptoms. Common medications for PAD may include:
- Antiplatelet agents: Medications like aspirin or clopidogrel help prevent blood clots and reduce the risk of complications.
- Cholesterol-lowering medications: Statins are often prescribed to lower LDL cholesterol levels and reduce the risk of atherosclerosis progression.
- Blood pressure management: Medications to control high blood pressure, such as ACE inhibitors or beta-blockers, may be prescribed to reduce strain on the arteries.
- Medications to control diabetes: For patients with diabetes, maintaining good blood sugar control is important to minimize the impact on blood vessels.
3. Interventional Procedures: In more severe cases of PAD, doctors may recommend interventional procedures to restore blood flow. These may include:
- Angioplasty: A minimally invasive procedure where a balloon catheter is used to widen narrowed or blocked arteries.
- Stenting: In some cases, a stent (a small mesh tube) is placed in the artery to help keep it open and improve blood flow.
- Bypass surgery: In advanced cases, bypass surgery may be necessary to create a new route for blood flow by using a graft to bypass the blocked artery.
It’s important to note that treatment plans are individualized based on each patient’s specific condition, medical history, and overall health.
